If you’re considering a dental bridge to replace missing teeth, you may wonder, “Do dental bridges damage surrounding teeth?” This is a valid concern many patients raise before committing to treatment, and it deserves a thoughtful answer grounded in evidence and clinical experience.
When placed by a registered dentist and maintained properly, dental bridges can function well for many years. They require preparation of adjacent teeth, and individual outcomes vary. Bridges do require modification of adjacent teeth to support the restoration, and they demand diligent ongoing care. The preparation process is a controlled, intentional reshaping performed by your dentist. The key difference lies in several critical factors: proper placement technique, bridge design and fit, individual oral hygiene practices, and regular professional monitoring.
In this guide, we’ll explore how a dental bridge interacts with surrounding teeth, gum tissue, and bone. You’ll learn about the effects on supporting teeth and understand potential complications and prevention. You’ll also discover maintenance practices that may support ongoing oral health with a dental bridge. This information can help you have an informed conversation with your dentist about whether a bridge is appropriate for your circumstances.
Contents Navigation
Summary of The Content
- Dental bridges require preparation of adjacent teeth to accommodate crowns, which represents an intentional modification rather than damage when performed by a dentist.
- The abutment tooth preparation process involves removing a thin layer of tooth structure, which is irreversible but typically doesn’t compromise the tooth’s long-term viability with proper care.
- Gum recession around bridges can occur due to poor fit, inadequate hygiene, or natural ageing. Proper maintenance and regular monitoring may help reduce these risks, though outcomes vary.
- Bridges don’t stimulate jawbone tissue the way natural teeth or implants do, and some bone loss naturally occurs after tooth loss, regardless of bridge placement.
- Thorough daily cleaning and regular professional care may help reduce the risk of these issues, though they cannot be entirely prevented.
- Proper bridge maintenance requires specific cleaning techniques, such as floss threaders, interdental brushes, or water flossers, to access areas beneath the pontic and around crown margins.
How Dental Bridges Interact With Adjacent Teeth
Dental bridges are anchored to adjacent teeth, which are called abutment teeth. These supporting teeth must be prepared or trimmed to accommodate crowns that hold the bridge in place. This represents a modification of the tooth structure rather than damage in the traditional sense.
Understanding this distinction is important when asking, “Do dental bridges damage surrounding teeth?” The reshaping is intentional and controlled, designed to create a proper fit and function for the restoration. This differs from the unintended harm that might result from complications such as decay or infection. Current dental bridge techniques aim to preserve healthy tooth structure whilst providing the support needed for the bridge to function.
The preparation process follows established protocols that balance the need for adequate crown retention with tooth preservation. Your dentist removes only what is necessary so the bridge fits properly and functions well during chewing and speaking. The way bridges affect adjacent teeth depends largely on the quality of this preparation and the ongoing care you provide. Proper maintenance may help reduce the risk of complications such as decaying teeth under the bridge. This can affect the longevity of both the restoration and supporting teeth.
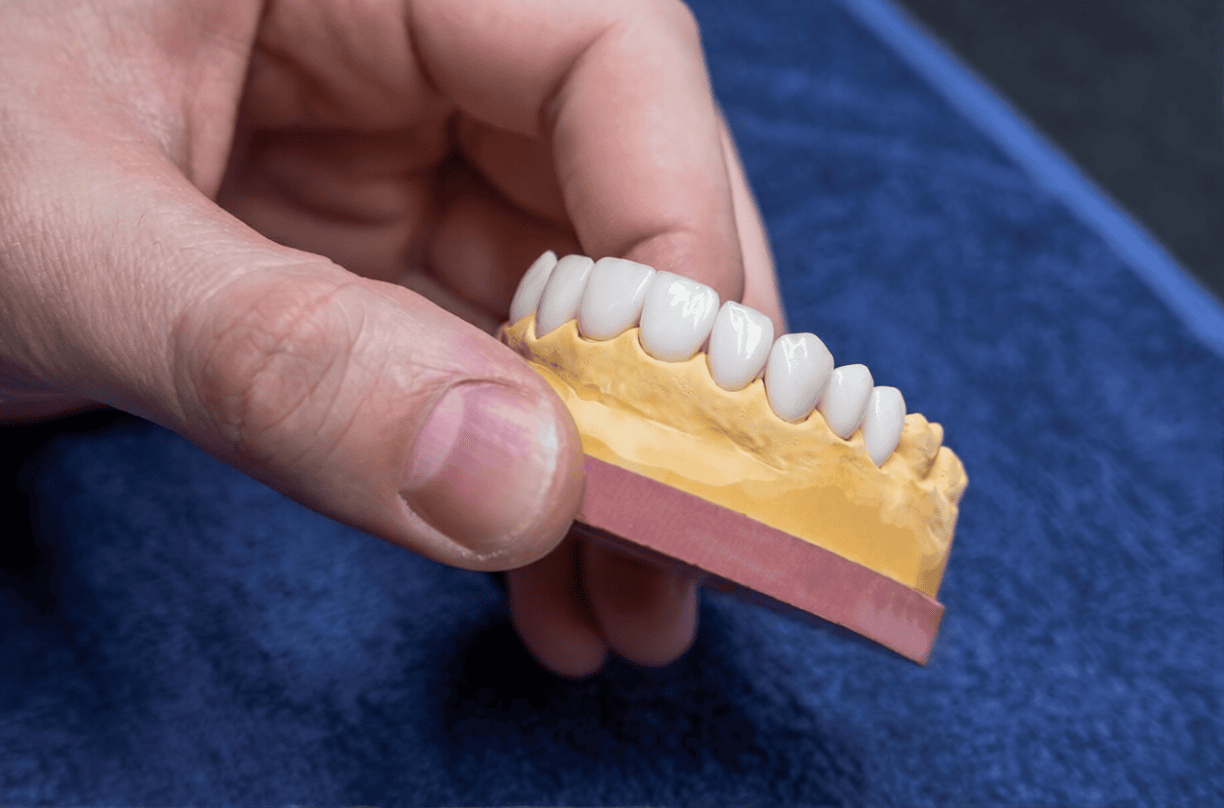
The Abutment Tooth Preparation Process
During bridge preparation, your dentist removes a thin layer of tooth structure from the supporting teeth. This creates space for the crowns that will anchor the bridge. The removal involves both enamel (the outer protective layer) and some dentine (the layer beneath enamel).
This removal is irreversible, which means the prepared teeth will always need a cover, either from the current bridge or replacement crowns in the future. Understanding the health of the abutment teeth is essential when considering this treatment, as the preparation represents a change to your natural teeth.
When performed by a dentist, this preparation represents an irreversible modification. With proper care and monitoring, prepared teeth can remain functional, though individual outcomes vary.
Long-Term Effects on Supporting Teeth
Research and clinical experience indicate that abutment teeth may remain healthy for many years when bridges are well maintained and properly fitted, though individual outcomes vary. The long-term success of supporting teeth depends largely on factors within your control, such as daily hygiene practices and regular dental visits.
Common concerns about bridges harming supporting teeth are often due to poor hygiene or ill-fitting bridges, rather than the bridges themselves. When bridges fit well, and patients maintain thorough cleaning routines, supporting teeth can remain functional, though individual outcomes vary and complications may occur despite proper care. The question of how long bridges last often depends on how well the supporting teeth are maintained.
Monitoring the health of abutment teeth through regular dental examinations allows your dentist to detect early signs of concern before they develop into more serious issues. Regular check-ups can detect early signs of decay under the bridge, enabling prompt intervention. Many patients with bridges maintain healthy supporting teeth throughout the service life of the restoration. Dental bridge longevity often extends 10 to 15 years or longer with proper care, and the supporting teeth can remain healthy throughout this period.
Understanding the Impact on Gum Health
The relationship between bridge margins and gums is critical to long-term oral health. Where the crown edges meet your gum tissue, careful design and placement help maintain healthy gums. While bridges require additional cleaning attention, proper maintenance techniques can help reduce the risk of gum disease and infection around the restoration.
Healthy gums around bridges can typically be maintained with appropriate care techniques and regular professional monitoring. Your dentist will show you specific techniques for cleaning around your bridge during the fitting appointment. These methods may feel unfamiliar at first, though most patients find them straightforward once they become part of the daily routine. Proper cleaning may help reduce the risk of infection in the surrounding gum tissue.
Gum Recession Risks Around Bridges
Gum recession refers to the gradual exposure of tooth roots as gum tissue pulls away from the tooth surface. This can occur under certain circumstances around dental bridges, though it’s not an inevitable outcome.
Gum recession around bridges may happen if bridges are poorly fitted, with margins that irritate tissue and trigger inflammation. It can also occur if oral hygiene is inadequate, allowing plaque buildup that leads to gum disease. Additionally, natural ageing processes unrelated to the bridge can contribute to recession over time.
Not all patients experience gum recession around bridges. Proper bridge design with careful maintenance may help reduce this risk, though outcomes vary. When bridges are designed with smooth, well-adapted margins that sit at an appropriate level relative to the gum line, they may support gum health, though individual outcomes vary.
Preventing Periodontal Disease
Specific techniques help maintain healthy gums around dental bridges. Interdental brushes, small brushes designed to clean between teeth, can access the space beneath the pontic and around crown margins. Water flossers use a stream of pressurised water to remove debris from hard-to-reach areas. Floss threaders allow you to guide regular floss beneath the pontic to clean the gum line.
Regular professional cleanings may help reduce the risk of periodontal disease around bridges. During these appointments, your dentist or hygienist can access areas you may miss during home care and detect early signs of gum disease before they progress. Professional cleanings typically remove calculus (hardened plaque) that cannot be removed with home care alone.
Bone Health Considerations
Tooth loss and tooth replacement options affect the jawbone in different ways. Understanding these effects can help you make informed treatment choices and know what to expect over time.
Dental bridges don’t stimulate bone the way natural teeth or dental implants do. Natural tooth roots extend into the jawbone, where chewing forces stimulate the bone tissue and help maintain its density. When teeth are lost, this stimulation doesn’t continue, and some bone resorption (loss) typically occurs in the area of missing teeth. Bridges don’t prevent this natural process of bone loss with dental bridge placement, though they don’t typically accelerate it either.
Natural Bone Changes After Tooth Loss
Bone resorption occurs when teeth are lost because bone tissue requires stimulation from tooth roots (or implants) to maintain its density and volume. Without this stimulation, the body gradually resorbs the bone that previously supported the missing tooth.
This bone loss happens regardless of whether the space is filled with a bridge. It’s a biological response to the absence of tooth roots rather than a consequence of bridge placement. Bridges are designed to accommodate gradual changes in bone contour over time.
The rate and extent of bone loss associated with dental bridge placement vary among individuals, depending on factors such as age, overall health, and the location in the mouth. Front teeth typically experience less bone loss than back teeth because they bear less chewing force. Your dentist can monitor bone levels through periodic X-rays and adjust your bridge if significant changes occur.
How Bridges Differ From Implants for Bone Support
Dental implants are integrated into the bone, whilst bridges rest on top of gum tissue. This difference means implants may help maintain bone density in ways bridges cannot, though bridges offer other advantages.
Implants are titanium posts placed surgically into the jawbone, where they fuse with the bone tissue over several months. This integration allows implants to transmit chewing forces into the bone, potentially helping to preserve bone density in the area of missing teeth. Bridges, by contrast, transfer chewing forces to the supporting teeth rather than directly to the bone.
Bridges offer shorter treatment time because they don’t require surgical placement or the healing period needed for implant integration. They also don’t require sufficient bone density for placement, which can be an advantage for patients who have experienced significant bone loss when considering dental bridges.
Both options can be appropriate depending on individual circumstances. Treatment selection should be based on professional assessment of your bone condition, overall health, budget considerations, and personal preferences. Your dentist can discuss which option is most suitable for your situation and explain how each restoration interacts with surrounding tissues.
Potential Complications and Prevention
Like any dental treatment, bridges can occasionally develop complications, though many of these are preventable with proper care and early intervention. Awareness of potential issues enables early detection and treatment, which typically prevents minor concerns from becoming serious.
Understanding what can go wrong doesn’t mean these complications are inevitable or common. Rather, this knowledge helps you actively maintain your bridge and recognise when professional attention is needed. The question, “Do dental bridges damage surrounding teeth?” often relates to these preventable complications rather than the bridge itself.
Decay Risk and Nerve Sensitivity
The junction where bridges meet natural tooth structure, the margin, can be vulnerable to tooth decay under a dental bridge if plaque accumulates and isn’t removed through thorough cleaning. This consideration isn’t unique to bridges; any restoration requires careful hygiene at the margins.
Regular brushing, flossing, and professional cleanings may help reduce the risk of tooth decay under the bridge, though decay can still occur despite proper care. The crown covers most of the prepared tooth surface, but the margin where the crown meets the tooth remains exposed to the oral environment. Bacteria can accumulate in this area if cleaning is inadequate, potentially causing decay.
Tooth decay under a dental bridge often develops slowly and may not cause symptoms initially. This is why regular dental examinations are important—they allow your dentist to detect early decay before it compromises the tooth structure or requires extensive treatment.
During bridge preparation, significant amounts of enamel and dentine are removed from the supporting teeth. This can occasionally lead to nerve sensitivity or inflammation. Some patients experience temporary sensitivity to temperature or pressure after bridge placement, which may improve within a few weeks as the nerve adapts to the change. In some cases, sensitivity may persist and require further treatment.
Bridge Failure and Its Effect on Supporting Teeth
Bridge failure can occur through fracture of the bridge itself, loosening of the crowns from the supporting teeth, or loss of supporting tooth integrity due to decay or infection. How this affects the supporting teeth depends largely on how quickly the problem is addressed.
Prompt attention to bridge problems may help reduce the risk of damage to abutment teeth, though complications can occur despite timely intervention. If you notice your bridge feels loose or moves when you chew, contact your dentist straight away. Early intervention may allow re-cementing of a loose bridge or treatment of minor issues, though outcomes vary.
Delayed treatment of failing bridges can lead to more serious complications. A loose bridge may allow bacteria to enter the space between the crown and tooth, and lead to decay. Continued function with a damaged bridge can place abnormal forces on supporting teeth, potentially causing cracks or fractures.
Regular dental check-ups may help with early detection of issues with bridges, though problems can develop between appointments. Your dentist will examine the bridge for signs of wear, check that it remains firmly attached to the supporting teeth, and assess the health of the tissues around it.
Well-maintained bridges typically provide many years of service before replacement is needed. The lifespan of the bridge depends on factors such as the quality of the original placement, your oral hygiene practices, the forces placed on the bridge during chewing, and whether you maintain regular dental visits.
Proper Bridge Maintenance and Warning Signs
Proper maintenance is the single most important factor in preventing complications and preserving oral health around dental bridges. Whilst bridges require some cleaning techniques beyond normal brushing, most patients find that these techniques become routine quickly.
Your daily bridge care routine represents an investment in protecting both the restoration and the natural teeth supporting it. Thorough cleaning may help reduce bacterial buildup that can lead to gum disease and decay, supporting bridge function over time, though outcomes vary.
Regular professional monitoring complements your home care efforts. During dental examinations, your dentist assesses the bridge fit, the supporting tooth health, and the gum condition, identifying any concerns that need attention.
Daily Hygiene and Professional Care
Effective bridge care begins with proper brushing technique around crown margins. Use a soft-bristled toothbrush and fluoride toothpaste, angling the brush towards the gum line to clean where the crown meets the tooth. This area requires particular attention because it’s where plaque tends to accumulate.
Flossing around bridges requires special techniques because traditional floss cannot pass between the connected teeth. Floss threaders—thin, flexible tools that guide floss beneath the pontic—let you clean the gum line beneath the artificial tooth. Alternatively, a bridge floss with stiffened ends can be threaded under the pontic without additional tools.
Interdental brushes offer another effective cleaning method. These small brushes can access the space beneath the pontic from both the cheek and tongue sides, removing food particles and plaque that brushing alone may miss. Choose a size that fits comfortably in the space without forcing.
Water flossers provide an additional cleaning option, particularly useful for patients who find threading floss difficult. The pressurised water stream can remove debris from around crown margins and beneath the pontic. Whilst water flossers are helpful, they work alongside rather than replacing traditional flossing.
Regular dental examinations remain important for patients with bridges, typically every six months. Professional cleanings remove calculus that home care cannot eliminate, allowing practitioners to assess bridge fit and support tooth health and gum condition. Your dentist may recommend X-rays periodically to check for decay beneath crowns or changes in bone levels around supporting teeth.
Warning Signs Requiring Professional Attention
Certain symptoms indicate potential problems requiring prompt evaluation by a dentist. Being aware of these warning signs empowers you to seek timely care, which typically prevents issues from becoming serious.
Bridge movement or looseness represents an important warning sign. Your bridge should feel firmly attached and stable during chewing. If you notice any movement or if the bridge feels loose when you press on it with your tongue, contact your dentist promptly. A loose bridge may indicate that the cement has failed or that decay has compromised the supporting tooth structure.
Changes in how your teeth fit together when biting can signal bridge problems. If your bite feels different or if certain teeth seem to contact earlier than others when you close your mouth, this warrants evaluation. These changes might indicate bridge movement or settling.
Changes in the gum tissue around your bridge require attention. Redness, swelling, bleeding during cleaning, or visible recession of the gum line may indicate inflammation or infection. Whilst mild, temporary gum sensitivity can occur immediately after bridge placement, persistent symptoms suggest a problem that needs to be addressed.
Persistent bad odour or taste despite good hygiene can indicate trapped food debris or infection beneath the bridge. If you notice an unpleasant odour specifically around your bridge area, despite thorough cleaning, schedule a dental appointment for evaluation.
Pain or sensitivity in the supporting teeth may indicate a range of issues, from minor nerve irritation to more serious problems such as infection or decay. Any persistent discomfort in the teeth supporting a bridge should be evaluated promptly.
Some slight settling during the first few days after bridge placement is normal as you adjust to the new restoration. However, ongoing discomfort, movement, or other concerning symptoms should be reported to your dentist.
Early intervention may help address issues before they become serious, though outcomes vary. Don’t hesitate to contact your dental clinic if you notice any changes in your bridge or the tissues around it. Your dental team can assess the situation and recommend appropriate treatment to protect both your bridge and your natural teeth.
Can a Bridge Always Be Recemented? Understanding Limitations
Recementing is not always suitable, and understanding the limitations helps set appropriate expectations. The condition of the abutment tooth health plays a central role in determining whether recementing is appropriate. If the supporting teeth have developed decay, fractures, or structural compromise, recementing may not be the suitable approach.
The integrity of the bridge itself must be carefully evaluated. Bridges with cracks, worn margins, or damaged framework may not function adequately even after recementation. Your dentist will examine the bridge thoroughly to determine whether it remains structurally sound enough for reuse.
Diagnostic imaging provides important information about what’s happening beneath the bridge. X-rays can reveal decay, bone loss, or changes in the supporting teeth that may not be visible during visual examination alone. These findings significantly influence whether recementing can be considered.
The dental bridge lifespan varies from person to person, but bridges eventually reach a point where replacement becomes more appropriate than recementing. Factors such as how long the bridge has been in place, how much wear it has experienced, and whether your oral health has changed all contribute to this assessment.
Cement selection also matters. Some types of cement create stronger bonds than others, and the cement used during recementing must be appropriate for your situation. Your dentist will choose the cement based on the bridge material, tooth condition, and clinical requirements.
Bite forces and how your teeth come together affect long-term success. If your bite has changed or if you have habits such as grinding that place extra stress on the bridge, recementing alone may not address these functional concerns. Your dentist may discuss additional considerations in these situations.
It’s important to understand that even when all conditions seem favourable, recementing does not offer the same predictability as a new bridge. Recemented bridges may perform well for some time, but the length of service cannot be determined with certainty. Your dentist will discuss realistic expectations based on your clinical findings.
Final Thoughts
Dental bridges can be effective tooth replacement options that may support oral health when properly designed, placed, and maintained, though individual outcomes vary. They do require modification of supporting teeth and diligent ongoing care, though these considerations can be managed successfully by most patients.
Dental bridges present some challenges, particularly regarding cleaning techniques and long-term effects on bone. Appropriate care and regular professional monitoring may help manage these concerns, though outcomes vary. Cleaning methods become routine for most patients, and regular dental visits allow early detection of developing issues.
The question of whether bridges damage the teeth around them doesn’t have a simple yes-or-no answer. The outcome depends on multiple factors, including bridge quality, placement technique, your personal hygiene practices, and timely problem resolution. Many patients enjoy decades of successful bridge function whilst their natural supporting teeth remain healthy.
If you’re considering a dental bridge to replace missing teeth, we encourage you to book a consultation with Karrinyup Dental Centre for a personalised assessment. A professional evaluation is essential to determine whether a dental bridge is appropriate for your individual circumstances, taking into account your oral health, bone condition, budget considerations, and personal preferences. Your dentist can explain what to expect from treatment, demonstrate the cleaning techniques you’ll need, and develop an ongoing monitoring plan.