Is getting a dental bridge a good idea for your situation? The answer depends on several factors unique to you, including your oral health, budget, lifestyle, and long-term goals. Dental bridges are one way to replace missing teeth, but they’re not the only option and aren’t suitable for everyone.
This guide helps you evaluate whether bridges suit your individual circumstances by covering candidacy requirements, potential benefits, important limitations, alternative treatments, and costs. We’ll provide a framework to help you prepare for meaningful conversations with your dentist. However, individual suitability requires a professional dental assessment.
Contents Navigation
- Summary of The Content
- What Is a Dental Bridge and How Does It Work?
- Who May Be Suitable for Dental Bridges?
- Potential Benefits of Dental Bridges
- Important Considerations
- Comparing Bridges to Alternative Tooth Replacement Options
- What to Expect During the Dental Bridge Process
- Maintenance Requirements and Daily Care
- Making Your Decision: Questions to Ask and Framework
- Final Thoughts
Summary of The Content
- Dental bridges are prosthetics that replace missing teeth by anchoring to adjacent natural teeth, offering a non-surgical alternative to implants.
- Suitable candidates typically have one to three missing adjacent teeth, healthy supporting teeth, and good oral hygiene habits.
- Bridges can provide functional restoration for chewing and speaking, may improve smile aesthetics, and typically have shorter treatment timelines compared to implants.
- Bridges cost less upfront than implants but require eventual replacement, affecting long-term value calculations.
- Compared to implants, bridges avoid surgery but don’t preserve bone; compared to dentures, bridges offer greater stability but higher initial costs.
- Daily maintenance requires special cleaning techniques under the replacement tooth, adding approximately two to three minutes to oral hygiene routines.
- The decision depends on individual priorities, including budget, preferred treatment timelines, concerns about bone preservation, and willingness to alter healthy adjacent teeth.
What Is a Dental Bridge and How Does It Work?
A dental bridge is a secured prosthetic that replaces one or more missing teeth by spanning the gap between remaining natural teeth. Unlike removable dentures that you take out for cleaning, bridges are cemented in place. Unlike dental implants that integrate with your jawbone, bridges rest above the gum line and rely on adjacent teeth for support.
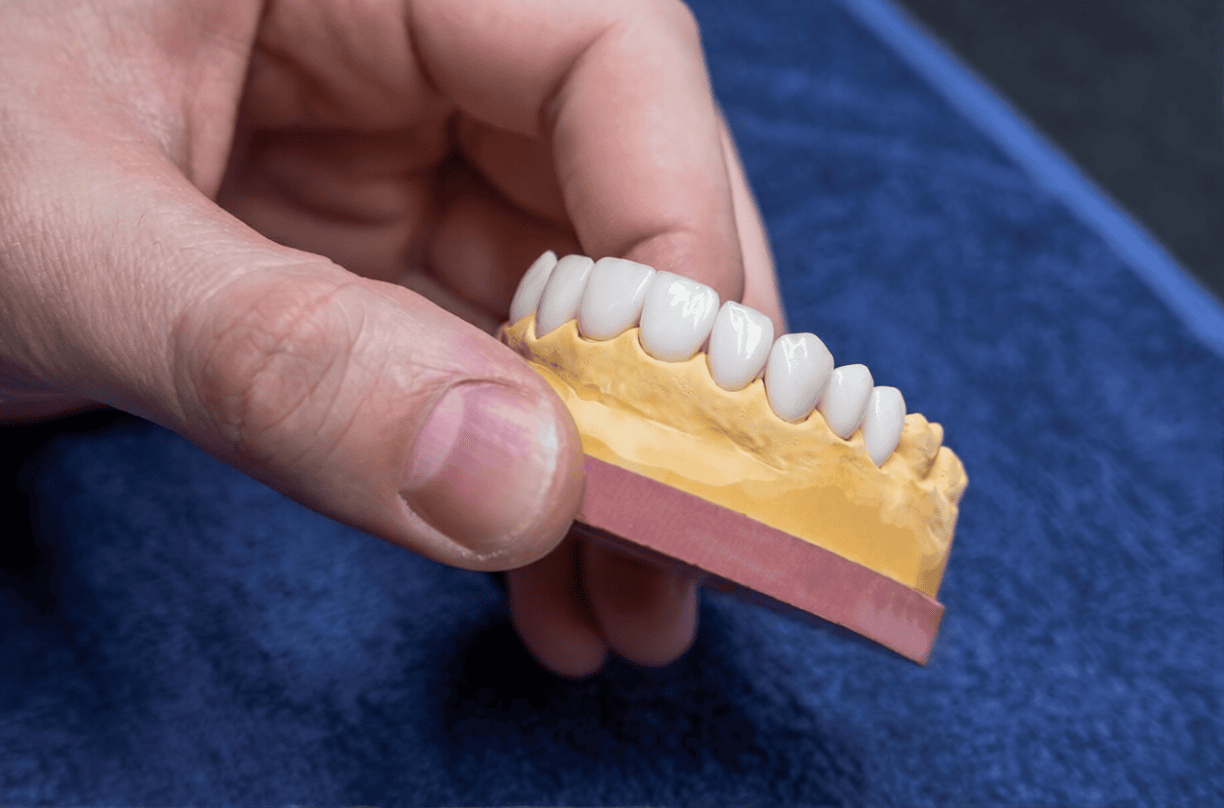
Dental bridges consist of three main components. The abutment teeth are the natural teeth on either side of the gap that support the bridge. These teeth are prepared with dental crowns that anchor the entire structure. The pontic is the artificial tooth (or teeth) that fills the gap where your natural tooth (or teeth) were missing. These components work together to form a stable, functional restoration.
There are four main types of dental bridges, each suited to different situations. Traditional bridges are the most common type, with crowns attached to abutment teeth on both sides of the gap. Cantilever bridges attach to an abutment tooth on only one side of the gap, used when teeth are present on just one side. Maryland bridges use metal or porcelain wings bonded to the back surfaces of adjacent teeth, requiring minimal tooth preparation. Implant-supported bridges are anchored to dental implants rather than natural teeth, combining the stability of implants with the efficiency of replacing multiple teeth in one restoration.
Who May Be Suitable for Dental Bridges?
Dental bridge candidacy depends on several factors related to your oral health and personal circumstances. You may be a suitable candidate for a bridge if several conditions apply. These include missing one to three adjacent teeth, having healthy teeth on either side of the gap, maintaining good oral hygiene, and having realistic expectations for outcomes and maintenance.
Bridges may be particularly suitable in several situations. These include when you can’t have implants due to insufficient bone density or medical conditions, when you prefer avoiding surgery, when budget constraints make implants difficult to afford, or when you need a relatively quick replacement option. Bridges may meet patient needs in these situations, though individual experiences vary.
However, dental bridge candidacy may be limited in certain circumstances. Very young patients whose jaws are still developing may need to wait for alternative options. Extensive tooth loss involving multiple non-adjacent teeth often requires different approaches. When the adjacent teeth are pristine and healthy, with no existing fillings or decay, your dentist may suggest alternatives that preserve them. Active gum disease needs to be addressed before bridge placement can proceed. If bone preservation is a priority for long-term oral health, your dentist may discuss other options that better support this goal.
Potential Benefits of Dental Bridges
Dental bridges can offer several benefits when they’re the right choice for your situation. Understanding these advantages helps you weigh them against limitations and compare bridges to alternative treatments.
Functional and Aesthetic Benefits
Bridges can help restore your ability to chew more comfortably. Speech clarity may improve as well, particularly if missing front teeth were affecting pronunciation. From an aesthetic perspective, bridges can help reduce the risk of surrounding teeth shifting towards the gap.
Patients typically need an adjustment period of one to two weeks after bridge placement. During this time, the bridge may feel slightly prominent, but many people adapt to their bridges.
Cost Comparison and Treatment Timeline
Understanding the value of dental bridges often involves comparing costs and timelines with those of alternative treatments. In Western Australia, traditional dental bridges typically cost between $3,500 and $6,500 per unit, depending on materials, complexity, and the number of teeth being replaced. Dental implants generally range from $4,500 to $7,500 per tooth, while partial dentures typically cost between $1,500 and $3,500.
The treatment timeline differs considerably between options. Bridges typically take two to four weeks from start to finish, requiring two to three appointments. This relatively quick timeframe appeals to patients who need timely tooth replacement. In contrast, dental implants usually require three to six months or longer due to the healing periods between surgical stages.
Payment plans may be available. Contact the clinic to discuss options if cost is a consideration.
Important Considerations
Whilst bridges offer benefits, it’s equally important to understand their limitations. Understanding dental bridge disadvantages helps you set realistic expectations and make choices aligned with your long-term oral health goals.
Lifespan and Replacement Considerations
Dental bridge longevity typically ranges from five to 15 years with proper care and maintenance. This compares to dental implants, which often last 20 to 25 years or longer, and partial dentures, which usually last five to seven years before needing replacement. These are general ranges, and individual experiences vary.
Several factors influence how long your bridge lasts. Oral hygiene quality plays a crucial role—thorough daily cleaning and regular professional check-ups help prevent complications that shorten bridge lifespan. Bite forces matter too; heavy grinding or clenching can wear down materials faster. Material selection affects durability, with porcelain-fused-to-metal and zirconia bridges generally lasting longer than all-porcelain options. Regular dental check-ups allow your dentist to monitor the bridge’s condition and address minor issues before they become significant problems.
Understanding dental bridge longevity helps with long-term planning. Your dentist can discuss realistic longevity expectations based on your specific circumstances, including bite patterns, oral health status, and lifestyle factors.
Impact on Adjacent Teeth
Traditional bridges require removing tooth structure from abutment teeth to accommodate the crowns that anchor the bridge. This preparation typically involves reducing tooth structure by approximately one to two millimetres on all surfaces. This process is irreversible—once tooth structure is removed, it cannot be replaced.
The implications of tooth preparation deserve careful consideration. Prepared teeth may become more vulnerable to sensitivity, particularly to temperature changes. If the bridge fails in the future or needs replacement, those abutment teeth will always require some form of restoration, even if you later choose a different treatment approach, such as implants.
Implant-supported bridges and Maryland bridges may minimise or avoid this concern. Maryland bridges require minimal preparation and bond to the back surfaces of adjacent teeth with small wings rather than covering the teeth entirely with crowns.
Bone Loss and Long-Term Oral Health
An important difference between bridges and implants relates to jawbone preservation. Unlike implants, bridges don’t prevent the gradual bone loss that occurs when tooth roots are missing. Understanding this process helps you evaluate long-term implications.
When natural tooth roots are present, they transmit chewing forces to the surrounding jawbone. This stimulation signals your body to maintain bone density in that area, much as exercise maintains muscle. When tooth roots are missing, this stimulation discontinues. Without it, bone gradually resorbs—your body redirects resources elsewhere because the bone appears unused.
This bone resorption can lead to several long-term consequences, though the extent varies considerably between individuals. Subtle changes in facial structure may occur over many years as bone volume decreases. Future implant placement may become more difficult if significant bone loss occurs, potentially necessitating bone grafting. In some cases, surrounding teeth may shift slightly as the supporting bone architecture changes.
Whilst this is one of the dental bridge disadvantages compared to implants, bridges may still meet patient needs when bone preservation isn’t their primary priority. The bridge vs implant comparison often comes down to weighing these different priorities.
Comparing Bridges to Alternative Tooth Replacement Options
No single tooth-replacement option is right for everyone. Your choice depends on individual priorities, oral health status, budget constraints, lifestyle factors, and long-term goals. This section provides balanced information to support productive discussions with your dentist.
Dental Bridges vs. Dental Implants
The bridge vs implant comparison involves multiple factors that matter differently to different patients. Understanding these differences helps you determine which aspects are most important for your situation.
When considering dental bridge longevity, bridges typically last five to 15 years with proper care, whilst implants often last 20 to 25 years or more. This difference in lifespan influences long-term planning and overall value calculations.
Bone preservation marks a significant distinction. Implants maintain jawbone density by replacing tooth roots and providing stimulation through chewing forces. Bridges don’t prevent bone loss in the gap area, which can have subtle long-term implications for facial structure and future treatment options.
Impact on adjacent teeth varies dramatically. Bridges require altering healthy adjacent teeth to accommodate supporting crowns, whilst implants stand independently without affecting neighbouring teeth.
Surgical requirements differ as well. Traditional bridges typically don’t require surgery—treatment involves tooth preparation and impressions. Implants require surgical placement into the jawbone, involving healing periods and associated considerations.
Implant-supported bridges combine aspects of both approaches, combining implants’ stability and bone preservation with bridges’ efficiency in replacing multiple adjacent teeth. It’s important to note that not all patients qualify as candidates for dental implants. Insufficient bone density, certain medical conditions, heavy smoking, or uncontrolled diabetes may limit implant suitability.
Dental Bridges vs. Partial Dentures
Comparing bridges to partial dentures involves different trade-offs than the bridge vs implant comparison. Partial dentures offer advantages and limitations.
Stability differs significantly. Bridges are secured in place, typically providing stable tooth replacement. Partial dentures are removable and can shift slightly during eating or speaking, particularly when first adjusting to them.
Comfort levels vary between patients. Bridges may feel more like natural teeth after the adjustment period, with many patients adapting well during daily activities. Partial dentures require adaptation time as well, and some patients remain aware of them long-term.
Maintenance requirements differ considerably. Bridges are cleaned like natural teeth, though special flossing techniques are needed to clean under the pontic. Partial dentures require removal for cleaning, soaking overnight, and careful handling to avoid damage.
Cost considerations favour partial dentures for upfront affordability. Partial dentures typically cost $1,500 to $3,500, considerably less than bridges. However, dentures usually need replacement every five to seven years, similar to or shorter than bridge lifespans. Long-term costs may become comparable.
Both options can provide natural-looking results when designed appropriately. Modern materials allow both bridges and dentures to look natural and blend seamlessly with existing teeth. Your dentist will consider factors like colour matching, tooth shape, and gum appearance.
Impact on adjacent teeth differs between these options. Traditional bridges require preparing adjacent teeth with crowns, whilst partial dentures typically use metal or tooth-coloured clasps that hook around existing teeth without major alteration. However, pressure from denture clasps can gradually affect supporting teeth over time.
The choice between bridges and partial dentures often depends on how many teeth you’re missing, your budget constraints, personal comfort preferences, and oral health status.
What to Expect During the Dental Bridge Process
The initial consultation begins with a comprehensive examination. Your dentist examines your teeth, gums, and bite pattern to assess suitability for a bridge. X-rays are taken to evaluate bone levels, tooth roots, and the condition of potential abutment teeth. During this appointment, your dentist discusses all available tooth replacement options, explains why they’re recommending a particular approach, and answers your questions. Treatment planning includes discussing costs, timelines, and what to expect throughout the process. This consultation provides the foundation for educated decision-making.
The tooth preparation appointment occurs once you’ve decided to proceed with a bridge. Your dentist administers a local anaesthetic to help manage discomfort during the procedure. They reshape the abutment teeth on either side of the gap, carefully removing a small amount of tooth structure to create space for the crowns that will support the bridge. Impressions are taken of your prepared teeth—these detailed moulds allow the dental laboratory to fabricate your custom bridge. A temporary bridge is placed to protect the prepared teeth and maintain function and aesthetics for one to three weeks whilst your new bridge is being made.
The final restoration placement appointment involves trying in your new bridge to check fit, appearance, and bite alignment. Your dentist makes any necessary adjustments for comfort and proper function. Once you’re satisfied with how the bridge looks and feels, it’s cemented in place.
Patients typically need one to two weeks to adapt to their new bridge. Initially, the bridge may feel slightly prominent or noticeable, particularly when eating or speaking. This is normal. Common early experiences include mild sensitivity to temperature in the prepared teeth and increased awareness when chewing. These sensations may diminish as you adjust. Your dentist will advise you to start with softer foods and may suggest gradually reintroducing your normal diet as you adapt.
Maintenance Requirements and Daily Care
Proper maintenance can influence how long your bridge lasts and help reduce the risk of complications. Bridge maintenance requirements involve daily care routines and regular professional monitoring.
Your daily routine should include brushing twice daily with fluoride toothpaste, paying particular attention to the areas where the bridge meets your natural teeth. Special cleaning is needed under the pontic (the replacement tooth portion). Food particles and plaque can accumulate in this area, causing gum irritation, decay in adjacent teeth, or unpleasant odours if not cleaned thoroughly. Use floss threaders or interdental brushes designed specifically for cleaning under bridges. Your dentist or hygienist can demonstrate proper technique during your appointment. Consider using an antimicrobial mouthwash to help reduce bacteria and support gum health.
Understanding why thorough cleaning matters helps motivate consistent habits. Plaque accumulation under the bridge and around abutment teeth can cause decay in the supporting teeth, potentially compromising the entire bridge. Gum disease can develop if bacteria aren’t removed regularly, which leads to inflammation, discomfort, and potential bridge failure. Food trapped under the bridge can cause irritation and bad breath.
Additional bridge maintenance requirements include attending six-monthly dental check-ups for professional cleaning and examination. During these visits, your dentist monitors the bridge’s condition, checks for signs of wear or damage, and can address minor issues before they become significant problems. Avoid biting into very hard foods, such as ice, hard lollies, or bones, as this can chip or crack the bridge materials. Sticky foods like toffee or caramel can pull at the bridge or get stuck underneath it. If you grind or clench your teeth at night, your dentist may recommend a nightguard to protect the bridge from excessive forces.
Once you’ve learned the technique, bridge maintenance requirements typically add about two to three minutes to your daily oral hygiene routine. Many patients find this manageable as part of their oral care routine to preserve their bridge and support oral health.
Making Your Decision: Questions to Ask and Framework
Preparing for your consultation with thoughtful questions helps you gather the information needed for decision-making. This section provides key questions to ask and a framework for evaluating your priorities.
Consider asking your dentist these important questions during a consultation. First, am I a suitable candidate for a dental bridge, and what alternatives might work for my situation? Understanding your options thoroughly helps you compare them. Ask which type of bridge they recommend and why—the rationale behind their recommendation reveals their clinical thinking.
Enquire specifically about what preparing the adjacent teeth involves and whether this concerns them, given the teeth’s current condition. How long can I expect this bridge to last, and what factors might affect its longevity?
Request detailed information about total costs, including the bridge itself, any preliminary work needed, and ongoing maintenance, as well as available payment options. Check whether your health fund provides cover and what out-of-pocket expenses you should anticipate.
Ask about maintenance requirements and what daily care routine you’ll need to follow. What should I expect during the adjustment period, and what’s considered normal versus concerning? Request information about warning signs that something’s wrong with the bridge—when should you contact the clinic? Finally, ask what options exist if the bridge fails or needs replacement in the future, and how that affects the supporting teeth in the long term.
A practical decision framework can help you evaluate the answer to “Is getting a dental bridge a good idea?” for your specific circumstances. Consider these key factors as you weigh your options.
Clinical suitability comes first. Do you meet the health requirements for a bridge? Are your adjacent teeth healthy enough to support it? Does your dentist believe a bridge is clinically appropriate? If there are clinical concerns, other options may serve you better.
Financial considerations matter for most patients. Can you afford the upfront cost of a bridge, or would payment plans make it manageable? How does the bridge cost compare to alternatives, and how does longevity factor into long-term value? What does your health fund cover, and what are the out-of-pocket expenses?
Longevity expectations influence your decision. Are you comfortable with a lifespan of 5 to 15 years, or do you prefer investing in something that typically lasts longer? Does the need for eventual replacement concern you significantly?
Lifestyle factors include your willingness to commit to thorough daily cleaning, including the special flossing techniques needed. Are you comfortable with dietary modifications to protect the bridge? Do you have habits, such as teeth grinding, that might require additional protective measures?
Personal priorities vary considerably between patients. Is minimising upfront cost your primary concern, or are you willing to invest more for longer-lasting results? Do you prefer quick treatment and avoiding surgery, or are you comfortable with longer timelines and procedures if they offer other benefits? How important is preserving your adjacent teeth in their current state? Does bone preservation matter significantly for your long-term planning? How do aesthetics in your smile rank in your priorities?
There’s no single “right” answer—your choice depends on which factors matter most to you. Some patients prioritise affordability and quick treatment, making bridges a suitable option. Still others prefer avoiding any alteration to healthy teeth, potentially choosing partial dentures.
Final Thoughts
Dental bridges can be a suitable tooth replacement option for many patients, potentially offering functional improvements, aesthetic benefits, and relatively quick treatment timelines. They may help restore your ability to chew more comfortably, improve the appearance of your smile, and help maintain proper tooth positioning. For patients who can’t have implants, prefer avoiding surgery, or need cost-effective tooth replacement, bridges may provide benefits.
However, the answer to the question, “Is getting a dental bridge a good idea?” ultimately depends on your individual circumstances. Your oral health status, budget constraints, lifestyle factors, and personal priorities all influence whether bridges align with your needs and goals. Important considerations include the finite lifespan requiring eventual replacement, the irreversible alteration of adjacent teeth, and the fact that bridges don’t prevent bone loss in gap areas. These limitations matter differently to different patients.
Use the decision framework and questions provided in this guide to prepare for productive consultations with your dentist. Discuss your specific situation openly, share your concerns and priorities, and ask for clarification about anything you don’t fully understand. Your dentist can assess your candidacy, explain which options suit your circumstances, and help you evaluate trade-offs between different approaches.
If you’d like to discuss whether dental bridges are suitable for your situation, contact Karrinyup Dental Centre to arrange a consultation. Our team can assess your individual needs and discuss all available tooth replacement options with you, providing the personalised information you need to make a decision.
Remember that individual suitability requires professional assessment. This article supports informed decision-making by providing comprehensive information about bridges, but it doesn’t replace personalised advice from a registered dental practitioner who can examine your specific oral health status and recommend appropriate treatment.